About
Foods for Special Medical Purposes (FSMPs) are evidence-based nutritional solutions for disease-related malnutrition and a wide range of other conditions in all ages. They can partially, or wholly, replace a normal diet to provide patients with the essential nutrients they need to survive, recover and thrive.
"Medical foods can enhance the quality of life for people with long-term conditions"
FSMPs are highly regulated and should be used under medical supervision across a wide range of settings such as hospitals, care homes, clinics and patients' own homes.
These foods include highly specialised feeds, oral nutritional supplements (ONS) or metabolic products, which can be taken orally or given as tube feeds. They can be a lifeline for patients of all ages, from infants (these specific products are referred to as infant FSMPs) to the elderly.
Patients requiring FSMPs range from those with food intolerance and inherited metabolic diseases, to those living with chronic illnesses. These may include cancer, cystic fibrosis, kidney failure or chronic obstructive pulmonary disease (COPD), diseases of the lung, muscular system or heart, as well as psychiatric and neurological conditions.
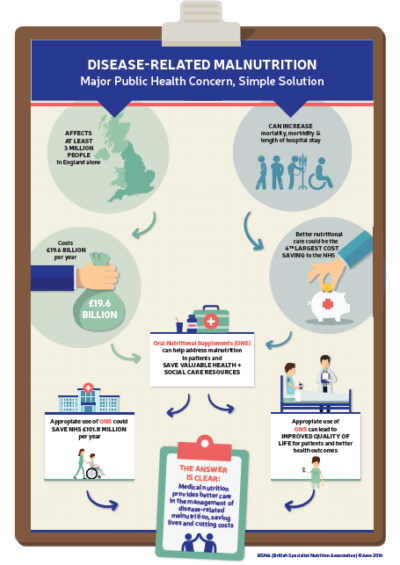
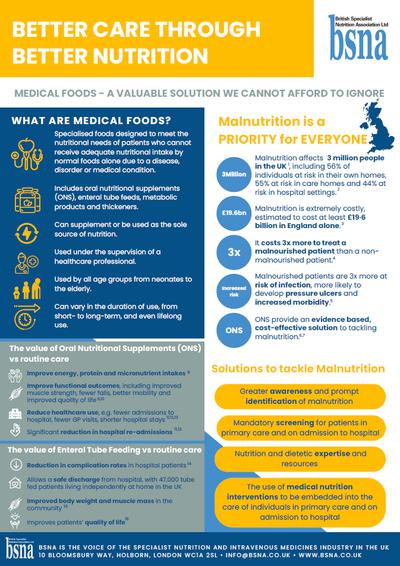
ONS can play an important role in supporting patients with malnutrition. Affecting at least 3 million people in the UK, the health and social expenditure for malnutrition is estimated at £19.6 billion per year in England alone. NICE has calculated that the delivery of better nutritional care could be the fifth largest potential cost saving available to the NHS.
- The NICE Quality Standard on Nutrition Support in Adults (QS 24) states that people who are malnourished or at risk of malnutrition should have a management care plan that aims to meet their complete nutritional requirements. QS 24 supports the NICE Clinical Guideline on Nutrition Support for Adults: oral nutrition support, enteral tube feeding and parenteral nutrition (CG 32)
- The NHS England Commissioning Guidance on Nutrition and Hydration (2015-2018) also recognises that malnutrition and dehydration have a large impact on the health economy with increased demands on GP services, out-of-hours services and increased rates of transition across pathways of care.
Person-centred nutritional care leads to positive health outcomes and reduces health and social care costs.
- The Value of Nutritional Care in Helping the NHS to Deliver on the NHS Outcomes Framework. An assessment on how nutritional care can enhance the quality of life for people with long-term conditions. The report can be downloaded here.
- Better Care Through Better Nutrition. An overview of how foods for special medical purposes (FSMP) can be a valuable solution to tackling disease-related malnutrition. A copy of the document can be downloaded here.
Enteral Nutrition
Enteral nutrition refers to feeding via the gastrointestinal tract, usually via a tube. It is required when patients are unable to meet a satisfactory nutritional intake from normal food due to a clinical condition, disorder or disease which has resulted in a difficulty swallowing or digesting solid food. Alternatively, patients may need to supplement their daily nutritional intake. Oral nutrition supplements (ONS) are a type of enteral nutrition.
Enteral nutrition can be provided by means of tube feeds or oral nutritional supplements.
- Tube feeds are usually administered directly into the stomach or gut, or via the nose. There is a wide variety of enteral feeds available for tube feeding. In addition to the products themselves, BSNA members provide the enteral feed and the equipment to assist in feeding and delivery.
- Oral nutritional supplements are taken predominantly via the mouth.
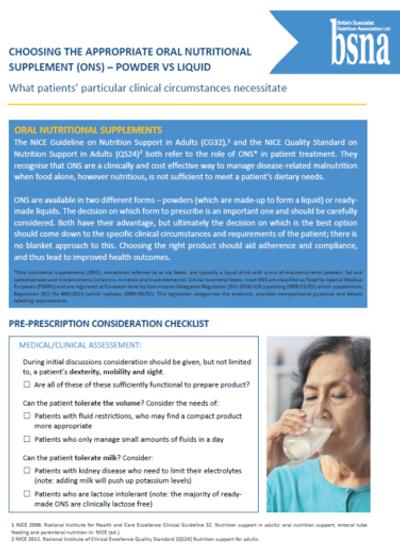
Oral Nutritional Supplements
ral nutritional supplements (ONS) are specialised foods designed to help meet the nutritional or dietary needs of patients living with a disease, disorder or medical condition who are temporarily or permanently unable to achieve an adequate nutritional intake from normal foods and are at risk of malnutrition.
ONS can partially, or wholly, replace a normal diet to provide patients with the essential nutrients they need when food alone is insufficient to meet their daily nutritional requirements. ONS should be used under medical supervision across a wide range of settings such as hospitals, care homes, clinics and in patients’ homes.
Most ONS are flavoured drinks which are sometimes called ‘sip feeds’. They are also available in dessert-, yoghurt-, soup- and savoury-style and as powders that can be made up into drinks and/or added to drinks or foods such as tea, coffee, custard and cereal. They are uniquely placed to deliver high calorie content and balanced nutrition in a single, easy-to-use serving: they have been designed and formulated to provide additional calories, protein and micronutrients (such as vitamins and minerals) to the diets of people who are either malnourished or at risk of malnutrition. They do not reduce intake of normal food. ONS are available in a variety of styles, volumes, flavours, textures and consistencies so that under the advice of their healthcare professional, patients can access the most appropriate product for their needs.
ONS are ready made or powdered products which are specially formulated to support patients with specific clinical requirements. They should only be used when clinically appropriate, as determined by a healthcare professional, for example:
- High protein ONS: usually for patients with wounds or fractures, post-operative patients, some types of cancer patients, renal patients on dialysis, COPD patients and the elderly
- Fibre-containing ONS: often used by patients with diarrhoea, constipation and neurological problems and patients on pain relief medication
- Pre-thickened ONS: for patients with conditions that affect their ability to swallow (dysphagia), such as stroke and neurological conditions
- Small volume, high energy dense ONS: usually for patients who cannot tolerate large volumes of food or drink
ONS and Malnutrition Management
The Managing Adult Malnutrition in the Community pathway is evidence based guidance developed by healthcare professionals and is supported by organisations such as the Royal College of General Practitioners (RCGP), the Royal College of Nursing (RCN) and the British Dietetic Association (BDA). It clearly sets out how ONS should be prescribed and used alongside food to manage disease-related malnutrition. It also provides guidance on how to monitor use of ONS and when to discontinue it.
The provision of dietary advice and ONS to malnourished patients reduces complications such as infections and wound breakdown by 70% and mortality by 40%. The use of ONS is linked to reduced hospital stay, which is the main driver of potential cost savings to the NHS. The reduced burden on healthcare services, as a result of ONS use, amounts to a potential total cost saving of £101.8 million per year in England alone. When ONS are used for 3 months or more amongst patients in the community and care homes, the median cost saving is 5%, as well as improved clinical outcomes such as improved quality of life, reduced infections, reduced minor post-operative complications, reduced falls and improved functional limitations.
Cost-effective benefits of ONS (YouTube)The Value of Oral Nutritional Supplements
An overview of how oral nutritional supplements (ONS) can help combat disease-related malnutrition can be downloaded here.

Infant FSMPs

Infant FSMPs (iFSMPs) are made specifically for infants who have special dietary requirements associated with a disease, disorder or medical condition that may be difficult or impossible to manage through breastmilk or the use of infant formula alone.
These conditions include, but are not limited to, allergies and intolerances, disturbance in amino acid or fatty acid metabolism, digestive disorders, fat malabsorption, malnutrition, cystic fibrosis, epilepsy, galactosaemia, liver failure and kidney failure. In addition, there are FSMPs for infants intended for the dietary management of infants born prematurely and iFSMPs available to manage clinical conditions, for example extensively hydrolysed formulae for infants and children with Cow’s Milk Protein Allergy, or amino acid feeds for children with severe or multiple food allergies. These pre-digested feeds also have an invaluable role to play in the management of diseases of the gastrointestinal tract, e.g. Crohn’s disease or post gastro surgery.
Some of the most widely used FSMPs designed for infants and children are high energy feeds for infants who have faltering growth and/or increased calorie requirements due to their clinical condition. These feeds are nutritionally complete.
IDDSI
he International Dysphagia Diet Standardisation Initiative (IDDSI) came about to develop international standardised terminology and definitions for texture modified foods and thickened liquids for people with dysphagia, helping to improve patient safety.
The Framework consists of a continuum of eight levels (0-7) and includes descriptors, testing methods and evidence for both liquid thickness and food texture levels.
In October 2017, IDDSI was adopted in the UK by The British Dietetic Association (BDA) and Royal College of Speech and Language Therapists (RCSLT) and on 1 April 2018 the transition to implement the IDDSI Framework in the UK began. Over the next 12 months, manufacturers will be updating their dysphagia product labels in line with the IDDSI descriptors. It is important to note that products will transition at different times over the next 12 months.
Click here to see when manufacturers are planning on updating their labels. Please note that these dates are subject to change.
By April 2019, IDDSI will be fully implemented across all healthcare settings.
* Please note, the IDDSI descriptors are only applicable for pre-thickened ONS and thickeners